Translate this page into:
A case report of peripheral T-cell lymphoma presenting as autoimmune hemolytic anemia
*Corresponding author: Jayasree M. Govindan, Department of Pathology, Vayalil Parambath Shamsheer Lakeshore, Hospital and Research Centre, Eranakulam, Kerala, India. jayagovindan@rocketmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varghese SS, Govindan JM. A case report of peripheral T-cell lymphoma presenting as autoimmune hemolytic anemia. J Hematol Allied Sci. 2025;5:90-2. doi: 10.25259/JHAS_59_2024
Abstract
A case of autoimmune hemolytic anemia (AIHA) with pancytopenia was presented to our institute as the peripheral center found difficulties with cross-matching and transfusion. Flow cytometry of peripheral blood, lymph node biopsy with immunehistochemical studies, and T-cell receptor gene assay confirmed peripheral T-cell lymphoma not otherwise specified (PTCL-NOS). Peripheral T-cell lymphoma most often presents with enlarged lymph nodes and paraneoplastic features such as eosinophilia and pruritus; however, AIHA could be a rare manifestation. With initiation of chemotherapy, though the patient has recovered well, later on succumbed to COVID. The literature shows that PTCL-NOS can have varied some even rare clinical presentations and requires a multimodality approach for making a conclusive diagnosis.
Keywords
Hemolytic anemia
Lymphoma
T-cell
Peripheral
INTRODUCTION
Peripheral T-cell Lymphoma, not otherwise specified (PTCL-NOS), which accounts for only 10–15% of all lymphoid malignancies is a heterogeneous group of nodal and extranodal mature T-cell lymphomas that do not correspond to any of the specifically defined entities of mature T-cell lymphomas.[1,2] Peripheral T-cell lymphoma (PTCL) usually presents as peripheral lymphadenopathy with B-symptoms and could present in advanced stages probably with involvement of bone marrow, liver, and spleen. Paraneoplastic features such as eosinophilia, pruritus and rarely hemophagocytic syndrome, sclerouveitis, cavity effusions, and autoimmune hemolytic anemia (AIHA) were also reported. They have a poorer prognosis compared to B-cell lymphoma.[3] During the maturation of lymphocytes, rearrangements of immunoglobulin gene segments occur, which can generate autoreactive lymphocytes and failure to eliminate them leads to autoimmune manifestations. AIHA appears to be independent of the stage of the disease.[4]
CASE REPORT
A 42-year-old woman was evaluated at multiple hospitals with anemia and found to have problems related to blood cross-matching as she had AIHA. She was referred to our institute for further management. She was found to have pancytopenia, elevated lactate dahydrogenase (LDH), uric acid, and increased D-dimer. Direct Coomb’s test and antinuclear antibody were positive. She soon developed bronchopneumonia and acute kidney injury and was initiated on antibiotics, non-invasive ventilator support, and multiple blood transfusions. She was also found to have multiple subcentimetric lymph nodes. Peripheral blood smear showed features of AIHA with atypical lymphoid cells and eosinophilia which, on Flow cytometry, showed a clonal proliferation of cluster of differentiation (CD)3 and CD5 positive with downregulated CD 7 T-cells showing CD4 predominance [Figure 1]. Concurrent bone marrow biopsy revealed para-trabecular infiltrates of atypical lymphoid cells.
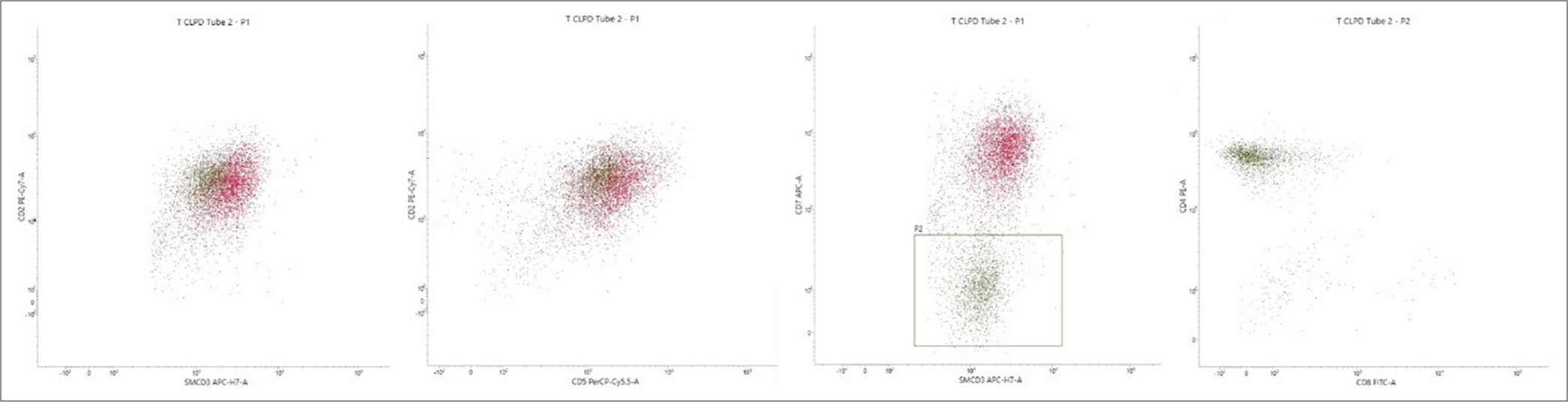
- Flow cytometry from peripheral blood shows a population of mature lymphocyte events in plot 1 high lighted by the T lymphocyte markers CD2 and Surface CD3 in subsequent plots are showing positive expressions for CD5 A population of events are CD7 downregulated and these are CD4 positive clonal t cells CD cluster differentiation APC, PECY 7 APC H7, PERCP and V450 are the various flourochrome conjugates used for identification.
Soon, she developed acute inflammatory demyelinating polyneuropathy and multiorgan dysfunction syndrome and was treated with intravenous immunoglobulin. Cerebrospinal fluid cytology showed atypical lymphoid cells. Since her condition was deteriorating and no reason identified, lymph node biopsy was suggested. Nevertheless, she was not stable enough for an excision biopsy; lymph node biopsy done at a previous center reported as reactive changes was reviewed. The hematoxylin and eosin showed marked expansion of paracortical region with diffuse small lymphoid infiltrate focally admixed with immunoblasts and focal clusters of dendritic cells with pigment [Figure 2]. These lymphoid cells were positive for CD3 and CD5, and CD7 negative with a dominant CD4 expression and a proliferation index of more than 70 [Figure 3a-d], an immune phenotype similar to what we found in the peripheral blood. Hence, we suggested PTCL-NOS as the diagnosis which was confirmed by T-cell receptor gene assay.
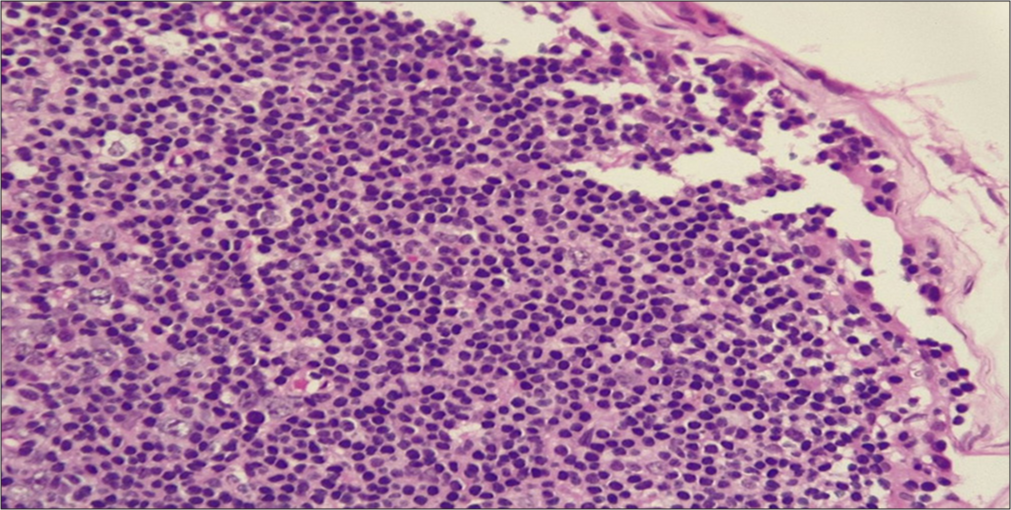
- Hematoxylin and eosin section from the lymph node ×40 magnification shows a diffuse paracortical infiltrate.
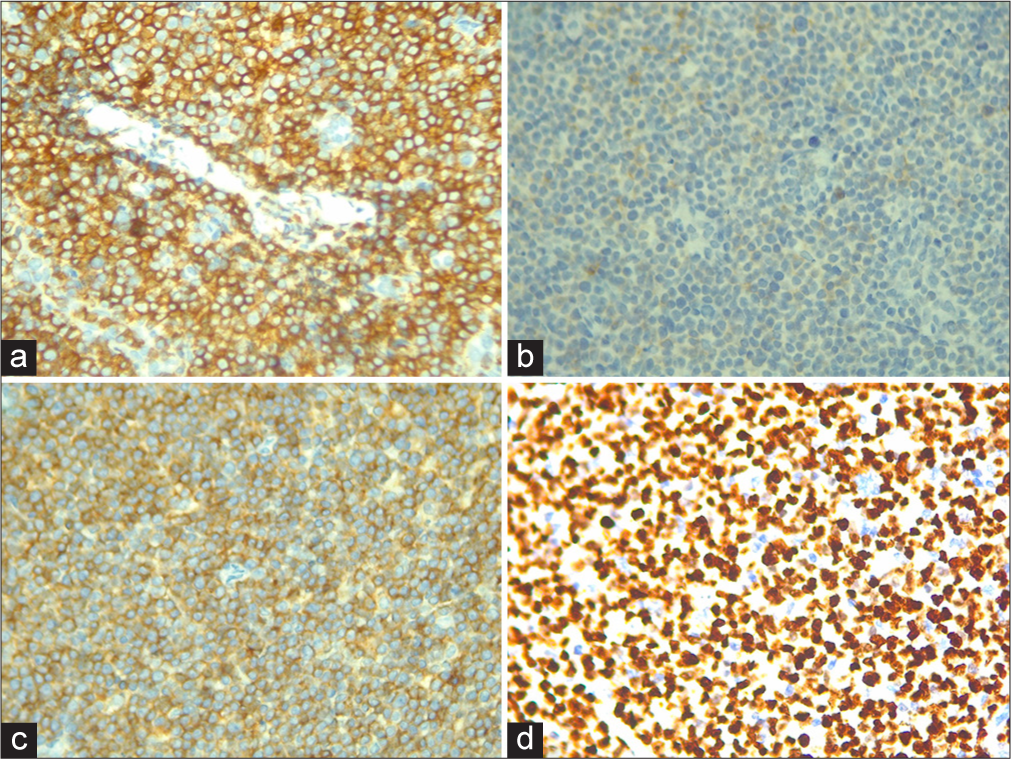
- (a) Immunohistochemistry (IHC) cluster of differentiation (CD)3, ×40 the paracortical infiltrate is composed predominantly of CD3 positive population of T lymphocytes. (b) IHC CD7, ×40 the paracortical infiltrate is negative for CD7. (c) IHC CD4, ×40 the paracortical infiltrate is composed predominantly of CD4 positive CD5 and population of T lymphocytes. (d) Ki67 proliferation index >70%.
The patient was started on chemotherapeutic drugs, cyclophosphamide, adriamycin, and prednisolone. Vincristine was withheld due to peripheral neuropathy. She had clinically improved and discharged; however, 6 months later came back with larger lymph nodes which, on biopsy, were suggestive of relapse that she was treated with the same regime and responded well. Unfortunately few months later, she passed away due to COVID-19 related complications.
CONCLUSION
AIHA is a rare, but known presentation in non-Hodgkin’s lymphoma. The histopathological diagnosis of PTCL can prove to be a challenge for many pathologists. However, a multimodality approach can guide the pathologists and clinicians to a conclusive diagnosis and prompt initiation of treatment.
Ethical approval
The research/study approved by the Institutional Review Board at LHRC, number LHRC/EC-2023101/16, dated 12th January, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Who classification of tumours of Heamatopoeitic and lymphoid Tissues, revised 4th ed IARC In: Lyon. 2017. p. :403-407.
- [Google Scholar]
- Peripheral T cell lymphoma: Clinico-pathological characteristics and outcome from a tertiary care centre in south India. Indian J Med Res. 2018;147:464-70.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral T-cell lymphoma: Review and updates of current management strategies. Adv Hematol. 2010;2010:624040.
- [CrossRef] [PubMed] [Google Scholar]
- Autoimmune hemolytic anemia in patients with nonHodgkin's lymphoma: Characteristics and significance. Ann Oncol. 2000;11:1571-7.
- [CrossRef] [PubMed] [Google Scholar]






