Translate this page into:
A case report on Pseudo Felty’s syndrome
*Corresponding author: Jayasree M. Govindan, Department of Pathology, Vayalil Parambath Shamsheer Lakeshore Hospital and Research Center, Ernakulam, Kerala, India. jayagovindan@rocketmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varghese SS, Govindan JM. A case report. J Hematol Allied Sci. 2024;4:120-2. doi: 10.25259/JHAS_58_2024
Abstract
Pseudo-Felty’s syndrome is a rare disease entity defined by the presence of monoclonal expansion of T lymphocytes with neutropenia in association with rheumatoid arthritis. T-large granular lymphocyte (LGL) leukemia is a lymphoproliferative disease with an indolent behavior. LGL leukemia arises in a setting of sustained immune stimulation, such as autoimmune disorders and chronic viral infections, where there is a clonal expansion of T-LGL (cluster of differentiation [CD]3+/CD8+) cells. In this article, we present the case of a 60-year-old gentleman with Pseudo-Felty’s syndrome who presented with LGL proliferation. He is presently stable on disease modifying anti-rheumatoid drugs including methotrexate.
Keywords
Autoimmune disorder
Large granular lymphocyte
Pseudo-Felty’s
Rheumatoid arthritis
INTRODUCTION
T-cell large granular lymphocyte (LGL) leukemia is a rare clonal hematologic disorder, which belongs to the category of chronic lymphoproliferative disorders of mature T/Natural killer cell (NK) cells. It is equally prevalent in both genders and occurs predominantly in adults in their fifth to seventh decade. It is rare in individuals <25 years of age. It is characterized by a persistent (>6 months) increase in the number of peripheral blood LGLs, usually to 2–20 × 109/L, without a clearly identified cause.[1-3] When associated with rheumatoid arthritis (RA), it is also known as Pseudo-Felty’s syndrome.
The clonal lymphocytes show moderate to abundant cytoplasm and fine or coarse azurophilic granules. These granules are positive for acid phosphatase and beta-glucuronidase. Ultrastructurally, the granules show parallel tubular arrays containing cytolytic proteins such as perforin and granzyme B.[2]
LGL leukemia is thought to be at the intersection of a clonal lymphoproliferative disease, chronic inflammation, and autoimmunity. The clonal T-LGLs are identical to normal cytotoxic T-lymphocyte effector memory cells, both phenotypically and functionally. Chronic stimulation by an unknown antigen, along with activating mutation of Signal transuducer and activator of trancription 3 (STAT3), and rarely STAT5B results in clonal expansion of LGL. This later on manifests as cytopenias and autoimmune diseases, like RA, which is attributed to the secretion of proinflammatory cytokines mediated by STAT3. In addition, there is increased circulating Fasligand, which induces neutrophil apoptosis and hence neutropenia.[3-5]
Felty’s syndrome, which is rare association with RA is defined by the presence of seropositive RA, splenomegaly, and neutropenia, the still rarer entity Pseudo-Feltys syndrome has a clonal T granular cell proliferation which should be confirmed by immune phenotyping.
CASE REPORT
A 60-year-old gentleman was referred to our hospital in view of unexplained persistent lymphocytosis. On examination, there was no lymphadenopathy and organomegaly. Blood counts were normal, with a differential count showing neutropenia and lymphocytosis, of which 5% transformed lymphocytes. Imaging of chest and abdomen was within normal limits. Peripheral blood film showed lymphocytosis where there were numerous large lymphocytes showing moderate amount of cytoplasm with coarse azurophilic granules (more than 60%) [Figure 1].
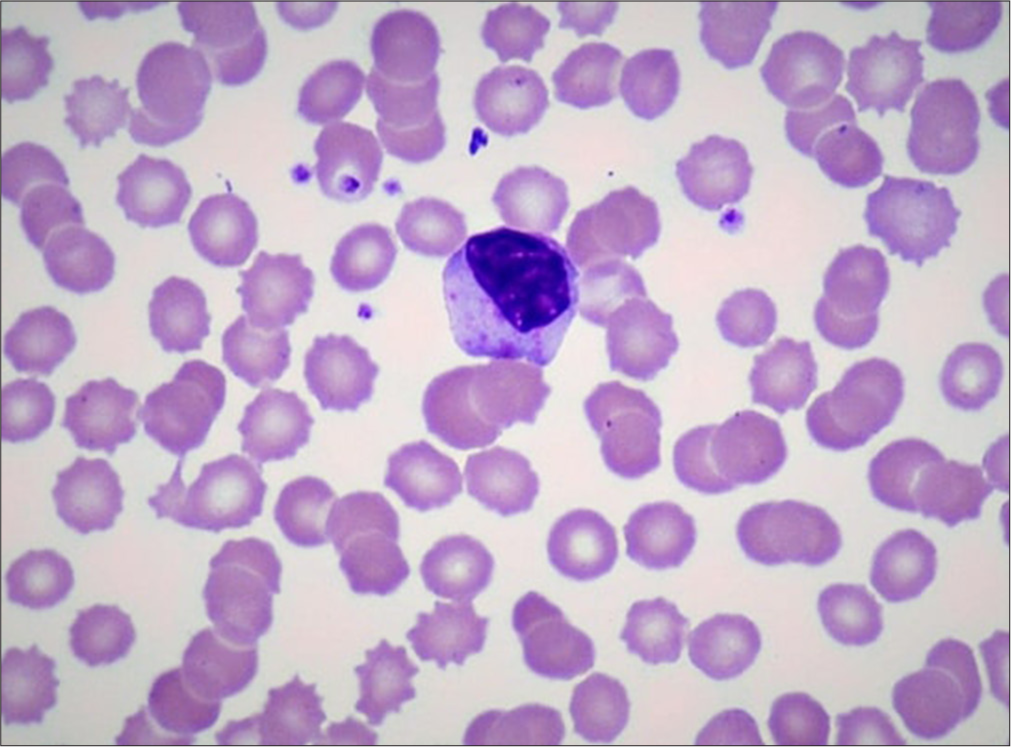
- It shows large granular lymphocytes in peripheral smear (oil immersion/×100, Leishman stain).
DISCUSSION
In view of the increased LG lymphocytes, we proceeded with flow cytometry. About 75% of the population was composed of lymphocytes, with a predominance of cluster of differentiation (CD)3+ T-cells. These cells showed dim expression of CD5 and CD7 with majority showing CD8 expression [Figure 2]. Thus, a diagnosis of LGL proliferation/leukemia was made. A suggestion to review the patient history was conveyed to the treating clinician.
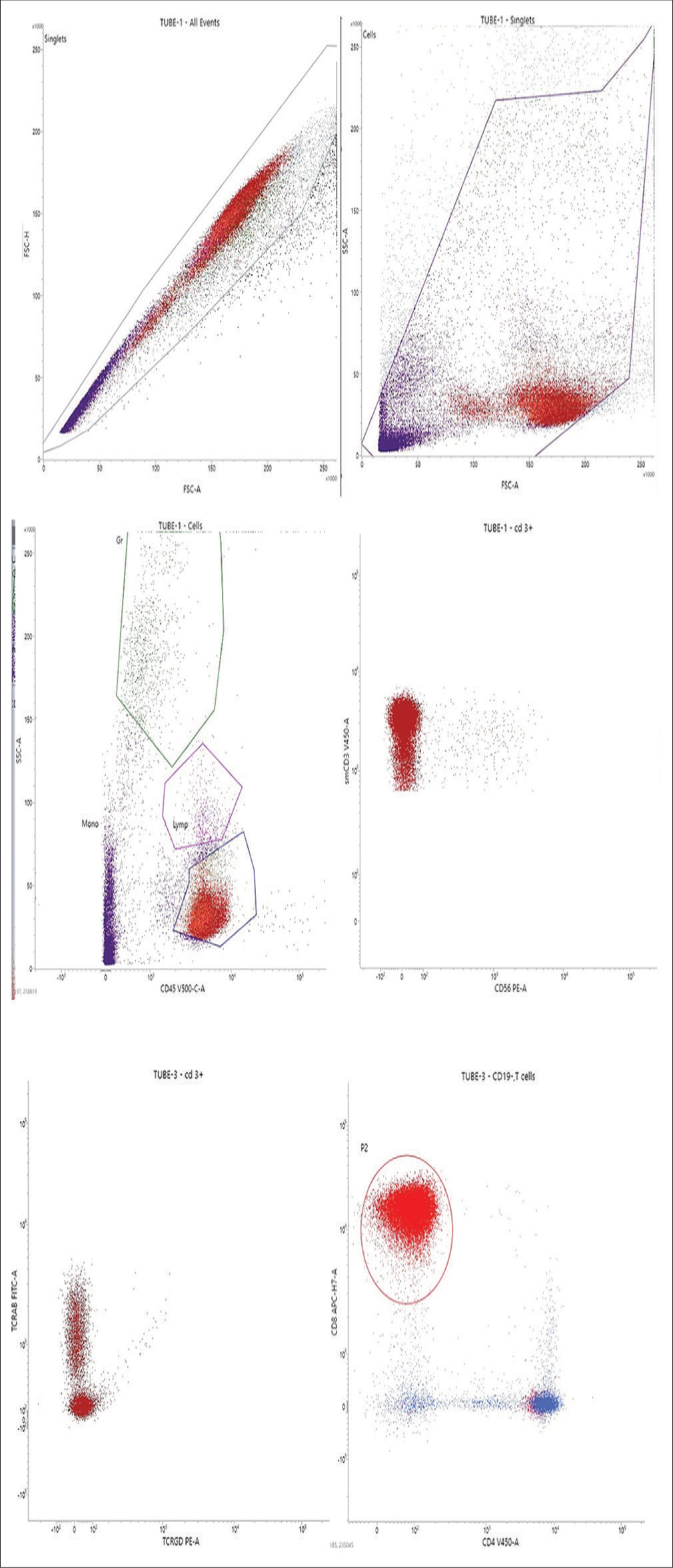
- Flow cytometry plots from the Peripheral blood with various cluster differentiation (CD) markers and TCell receptor alphabeta (TCRAB) TCell receptor gamma delta (TCRGD). The mature T cells showed uniform positivity for surface CD3 and CD8. The various flourochromes used for tagging are FITC: Flouroscine iso thiocyanate, PE: Phyco erythrine, APC: Allophycocyanine.
On reviewing the history, it was found that the patient was on disease modifying anti-rheumatoid drugs for RA for 2 years. Finally, the patient was diagnosed with Pseudo-Felty’s syndrome with T- LGL proliferation. On follow-up, the patient is stable.
CONCLUSION
RA is a systemic illness with numerous extra-articular manifestations. Proper treatment with regular follow-up is essential. LGL leukemia is a rare association seen with RA methotrexate which is the usual treatment modality for Feltys syndrome; however, Pseudo-Felty’s syndrome is less responsive. Clinical trials are under progress to develop targeted therapy, however limited by the lower number of cases.
Acknowledgments
We acknowledge the oncology department for referring the patient for evaluation.
Ethical approval:
The research/study approved by the Institutional Review Board at lakeshore hospital and research center, Kochi, number LHRC/EC2023/01/17, dated 12th January, 2023.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- T-cell large granular lymphocyte leukemia diagnosis in a patient with felty syndrome. Clin Med Rev Case Rep. 2017;4:188.
- [CrossRef] [Google Scholar]
- T-cell large granular lymphocytic lekemia: 4 cases. Blood Res. 2014;49:196-207.
- [CrossRef] [PubMed] [Google Scholar]
- T-cell large granular lymphocytic leukaemia In: Swerdlow SH, Campo E, Nancy LH, Jaffe ES, Pileri SA, eds. WHO classification of tumours of hematopoietic and lymphoid tissues (Revised 4th ed). Lyon: IARC; 2017. p. :348-50.
- [Google Scholar]
- Felty's syndrome autoantibodies bind to deiminated histones and neutrophil extracellular traps. Arthritis Rheum. 2012;64:982-92.
- [CrossRef] [PubMed] [Google Scholar]
- LGL leukaemia: From pathogenesis to treatment. Blood. 2017;129:1082-94.
- [CrossRef] [PubMed] [Google Scholar]






