Translate this page into:
Acute leukemia manifesting as a pericardial effusion in a pregnant female: A rare event
*Corresponding author: Gourik Gangopadhyay, Department of Pathology, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. gaurikgangopadhyay74@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gangopadhyay G, Gautam S, Siddiqui B, Rehman S. Acute leukemia manifesting as a pericardial effusion in a pregnant female: A rare event. J Hematol Allied Sci. 2024;4:114-6. doi: 10.25259/JHAS_36_2024.
Abstract
Pregnancy is an immunocompromised and hyperdynamic state. Although pregnancy makes a female vulnerable to a plethora of infections, primary malignancies in pregnancy constitute only about 0.1% of all malignant cases, out of which acute leukemias are relatively rare. Here, we present a case of acute leukemia presenting for the 1st time in pregnancy with the unusual manifestation of pericardial effusion. A 32-year-old patient, G3P2L2, presented to the obstetrics outpatient department of our hospital at 27 weeks with low-grade fever and dyspnea. Apart from other obstetric complications, radiological investigations confirmed pericardial effusion. Initial complete blood count revealed a markedly increased total leucocyte count of 88.9 × 103/mm3. Percutaneous pericardial drainage and peripheral blood film examination revealed a predominance of immature cells resembling blasts in both fluids. Pre-pregnant hematological records did not show any such abnormality. Chemotherapy was immediately commenced. However, the patient succumbed to acute leukemia. Due to its vague and nonspecific symptoms, the diagnosis of acute leukemia often poses an immense diagnostic dilemma, especially in early pregnancy. Even if diagnosed, chemotherapy needs to be administered with utmost precision to minimize adverse effects to the mother and fetus. Cases such as these need to be given due attention to consider leukemia as a possibility during pregnancy.
Keywords
Blasts
Chemotherapy
Effusion
Leukemia
Pregnancy
INTRODUCTION
Although pregnancy has been classically designated to be an immunocompromised state, the occurrence of malignancies during pregnancy is relatively uncommon, constituting only 0.07– 0.1% of all cases of malignant tumors.[1] The incidence of leukemia has been reported to be as low as 1 in 75,000–100,000 pregnancies, out of which two-thirds of the cases originate from the myeloid series, while only one-third are of the lymphoid lineage.[2]
The incidence of pericardial effusion in pregnancy has been reported to be 27.7 cases/100,000 person-years.[3] Most of the cases of pericardial effusion in pregnancy are secondary to acute or constrictive pericarditis. The common sites of infiltration of leukemia cells include lymph nodes, the spleen, and the central nervous system.[4] Pericardial infiltration of leukemia cells in acute myeloid leukemia (AML) is relatively rare, and only a few case reports have been recorded to date.
CASE REPORT
A 32-year-old patient, G3P2L2, presented to the Department of Obstetrics and Gynecology of Jawaharlal Nehru Medical College and Hospital (JNMCH), Aligarh Muslim University (AMU) with complaints of low-grade fever, dyspnea, pain in the jaw, and reduced fetal movement. She had a history of two lower-segment cesarean sections (LSCS) in the past, with cephalopelvic disproportion in both cases. She also mentioned a history of dog bites in the 2nd month of pregnancy, for which she received rabies vaccination as per the Essen regimen. Clinically, the patient was found to be having pallor 3+, pedal edema, blood pressure of 100/56 mm Hg, and muffled heart sounds but an audible S3. Ultrasonography revealed a singleton pregnancy with the fetus in breech. At the time of initial presentation, the gestational age was found to be 27 weeks 3 days, and the estimated fetal weight was 900 g. The amniotic fluid index was found to be only 2 cm, thereby indicating severe oligohydramnios. Furthermore, anomaly scans revealed multiple congenital anomalies in the developing fetus. Chest X-ray also revealed cardiomegaly along with pericardial effusion. Echocardiography done further confirmed the pericardial effusion.
Hematological investigations showed a hemoglobin of 4.6 g/dL, platelet count of 11000/mm3, and total leucocyte count (TLC) of 88.9 × 103/mm3. The serum electrolyte levels and kidney and liver function tests were within normal limits.
The dyspnea of the patient deteriorated dramatically within the first 48 hours of admission. Percutaneous pericardial drainage was done to relieve the condition. The peripheral blood and pericardial fluid was sent to the Department of Pathology, JNMCH, AMU. On microscopic examination of the peripheral blood, the red blood cell population showed anisopoikilocytosis and the platelet count was markedly reduced by smear. The TLC was found to be markedly raised, with as many as 80 immature cells having a high nucleo: cytoplasmic ratio, oval to round nuclei with fine nuclear membrane having prominent nucleoli and scant blue cytoplasm, thereby resembling myeloblasts [Figure 1]. Similar blasts resembling leukemic cells were also observed in the pericardial fluid sample. The blood smear was further stained with myeloperoxidase, yielding granular positivity. Thus, the provisional diagnosis of AML was established [Figure 2]. Flow cytometry and immunophenotyping were not available. Hematological records of the pre-pregnant state and initial pregnancy did not show any leukemic association.
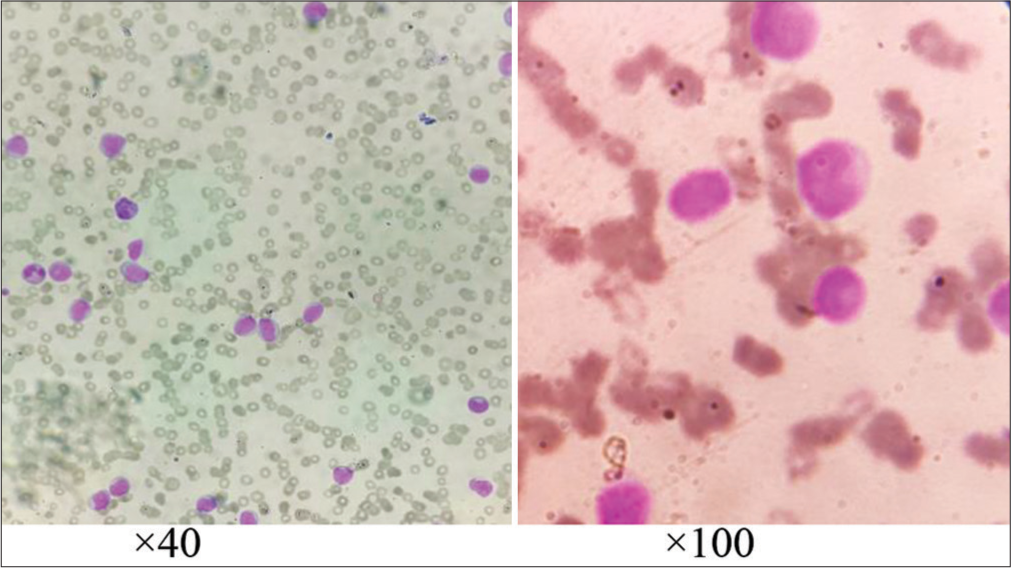
- Leishman stained peripheral blood smear shows multiple microcytic hypochromic red blood cells with predominance of immature cells having high nucleo: cytoplasmic, oval to round nuclei with fine nuclear membrane having prominent nucleoli and scant blue cytoplasm.
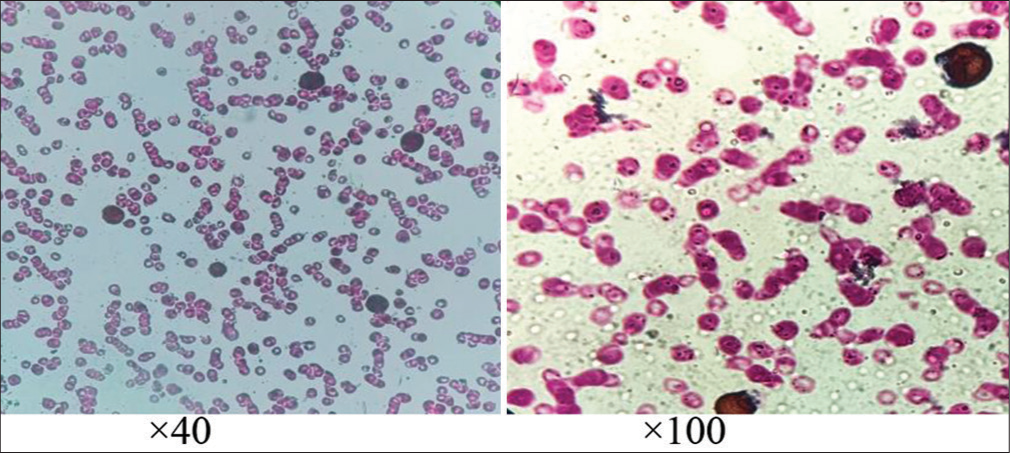
- Staining by myeloperoxidase showed diffuse granular positivity proving the immature cells to be myeloblasts.
The patient was further referred to the Department of Radiotherapy for management of the leukemic condition. She was initiated on daunorubicin and cytarabine arabinoside-based initiation therapy to address the AML. The decision was taken to terminate the pregnancy. Following the parenteral administration of dexamethasone, the patient was subjected to LSCS and a preterm baby was delivered.
The pregnancy was uneventful till the third stage of labor. However, after the delivery of the placenta, the mother suffered from mild post-partum hemorrhage. She developed early symptoms of puerperal sepsis on the 4th day following delivery. However, it was promptly controlled using parenteral antibiotics. The baby developed severe pathological jaundice. Attempts of phototherapy went in vain. He had to be subjected to a double volume exchange transfusion.
The condition of the patient deteriorated 2 weeks post-delivery. She developed severe pancytopenia. An echocardiogram revealed steadily increasing pericardial effusion. Eventually, the patient developed pyrexia of unknown origin, which could not be salvaged in spite of antibiotic therapy. The patient eventually succumbed to sepsis.
The baby continues to remain admitted in the neonatal intensive care unit at the time of writing this case report.
DISCUSSION
Acute leukemia poses an immense medical challenge during pregnancy. The non-specific symptoms and the physiological changes during pregnancy often masquerade and delay the diagnosis. Statistically, 23% of the acute leukemias in pregnancy are diagnosed in the first trimester, 37% in the 2nd trimester, and 40% in the 3rd trimester.[5] The treatment of leukemias is especially difficult in the first trimester during the period of organogenesis to achieve a viable outcome. Exposure to chemotherapy during the first trimester can lead to a 10–20% risk of major fetal malformation, especially if antimetabolites are added to the regimen.[6] A Spanish study computed the abortion rates to be 87%, 33%, and 7% for APML (M3 type of AML according to French American British Classification) diagnosed in the 1st, 2nd, and 3rd trimester, respectively.[7] A recent meta-analysis found the median survival rate of pregnant females diagnosed with AML to be 30%.[8] To arrive at a clear-cut management plan, the diagnostic possibility of leukemia should always be kept in mind in all cases of unexplained severe constitutional symptoms during pregnancy.
While small amounts of fetal pericardial fluid can be normally detected after 20 weeks of gestation, larger volumes of pericardial effusion in a pregnant female must raise suspicion toward rhesus isoimmunization, hydrops fetalis, hypoalbuminemia, autoimmune, and infective etiology.[9] The pericardial and pleural involvement by leukemic cells is an uncommon condition. In a retrospective cohort study involving 2592 leukemic patients from a single center, only 21% were found to be having pericardial effusion, the majority of which were trivial in size.[10] In post-mortem studies, only about 33% of cases of leukemia have been reported to be having cardiac involvement, 99% of which were asymptomatic.[11]
There have been only limited studies dealing with the prognosis of the development of pericardial effusion in patients with acute leukemia. Sampat et al. carried out a study involving 1600 patients diagnosed with acute leukemia (AML, acute lymphoblastic leukemia, or myelodysplastic syndrome) who developed pericardial effusion on an echocardiogram during the course of treatment. No significant difference in survival rate was perceived between patients of acute leukemia who developed pericardial effusion and those who did not.[10]
CONCLUSION
Our case report illustrates a relatively unfamiliar association of pregnancy with acute leukemia manifesting as pericardial effusion. Apart from the myriad of the more common pathological entities encountered during pregnancy, leukemias should always be kept among the differentials. Meticulous hematological workup and microscopic examination often serve as the initial clue to the diagnosis of such a condition.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cancer during pregnancy: The oncologist overview. World J Oncol. 2019;10:28-34.
- [CrossRef] [PubMed] [Google Scholar]
- Acute myeloid leukemia and pregnancy about a case and review of the literature. Sch Int J Obstet Gynecol. 2022;5:285-7.
- [CrossRef] [Google Scholar]
- Pericardial diseases in pregnancy. Can J Cardiol. 2023;39:1067-77.
- [CrossRef] [PubMed] [Google Scholar]
- Massive pericardial effusion and pleural effusion: Cardiac and pleural infiltration in newly diagnosed acute myeloid leukemia. J Egypt Natl Canc Inst. 2021;33:23.
- [CrossRef] [PubMed] [Google Scholar]
- Acute myeloid leukemia in the pregnant patient. Eur J Haematol. 2015;95:124-36.
- [CrossRef] [PubMed] [Google Scholar]
- Update on leukemia in pregnancy In: Leukemias-updates and new insights. London: InTech; 2015.
- [CrossRef] [Google Scholar]
- Acute promyelocytic leukemia during pregnancy: A systematic review of the literature. Cancers (Basel). 2020;12:968.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of pericardial effusions in patients with leukemia. Cancer. 2010;116:2366-71.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac infiltration as the first manifestation of acute lymphoblastic leukemia: A systematic review. Front Oncol. 2022;12:805981.
- [CrossRef] [PubMed] [Google Scholar]







