Translate this page into:
Central retinal artery occlusion in a young adult with sickle cell disease
*Corresponding author: Richa Surit, Department of Biochemistry, ISPAT General Hospital, Rourkela, Odisha, India. richasurit@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Surit R, Tiga A, Minz AM. Central retinal artery occlusion in a young adult with sickle cell disease. J Hematol Allied Sci. 2025;5:99-102. doi: 10.25259/JHAS_42_2024
Abstract
Sickle cell disease (SCD) is an autosomal recessive disease. Clinical presentation depends on mutation of hemoglobin protein. The complication due to SCD is variable, as it affects vascular bed of different organs due to accumulation of sickle hemoglobin in arteries. This vaso-occlusive event may affect vascular bed in the eye, causes sickle cell retinopathy. A 22-year-old female, known case of sickle cell anemia, presented with a sudden loss of vision in her left eye 2 days back with generalized myalgia for 5 days. The ocular examination revealed acute central retinal artery occlusion (CRAO). She underwent laboratory and radiological investigations. The blood investigations revealed normal biochemical parameters and normal coagulation profile. On ocular examination, the fundus fluorescein angiography revealed CRAO along with central serous retinopathy. This report advocates that the disease may result in life affecting complication like vision loss due to CRAO. This case indicates that only prompt management toward such cases will be beneficial for such patients. We need a proper approach for the management of SCD patients.
Keywords
Central retinal artery occlusion
Sickle cell disease
Young adult
INTRODUCTION
Sickle cell disease (SCD) is a hereditary anemia, which is result of homozygous mutation of hemoglobin gene. Its clinical presentation depends on mutation of hemoglobin gene. Sickle-cell anemia (SCA) is the name of a specific form of sickle-cell disease, in which homozygous mutation of hemoglobin gene occur and eventually cause formation of hemoglobin S (HbS), a sickle hemoglobin. Other forms of SCD are sickle-cell heterozygous, sickle cell combined with other hemoglobinopathies such as beta- or delta-thalassemia.
Sickle-cell anemia causes acute and chronic complications which affect the patient’s life. The important complication of SCA is the painful bone episode or vaso-occlusive event. The vasoocclusive event affects different organs in the body. One of them is involvement of eyes, which may lead to ocular complication. This may vary from non-proliferative eye disease to proliferative eye disease. These occlusions may be due to embolism in main retinal artery or its distal branches. These occlusive events may cause traction retinal detachment or vitreous hemorrhage and may result in vision loss if not treated timely.[1] The approximate incidence of central retinal artery occlusion (CRAO) is estimated to be around 1–2/100 000, which includes atherosclerosis and non-arteritic occlusions with predominance in older age groups but SCD in younger age groups.[2,3]
CASE REPORT
A 22-year-old female was presented to the emergency department with complains of generalized body pain for the past 5 days with loss of vision in the left eye. She complained that initially vision got blurred and then lost 3 days back. She had no history of accidental injury to her eyes or any drug toxication. She was diagnosed case of homozygous (SCA-HbSS and attended the other hospital for blood transfusion. Her last whole blood transfusion was done 2 months back. She was also taking hydroxyurea (500 mg OD) for the past 14 years.
On general examination, pallor was present, her blood pressure 90 mmhg systolic with 76 mmhg diastolic was recorded, and respiration rate was slightly raised, that is, 23 respiration per minutes. On systemic examination, auscultation of the heart and lungs were normal, with no hepatomegaly but splenomegaly was found (grade 1 [Hackett’s grading system]).
An ophthalmological examination was conducted by ophthalmologist and findings were tabulated [Table 1].
| Ophthalmological parameters | Right eye | Left eye |
|---|---|---|
| Vision | 6/6 | only perception of light with pupillary reflex defect |
| Intraocular pressure (NCT) | 15 mm Hg | 15 mm Hg |
| Anterior segment (conjunctiva, cornea, anterior chamber) | Clear, quiet | Clear, quiet |
| Pupil | Normal in size with normal pupillary reflex | Relative afferent pupillary defect – grade III |
| Lens | Clear | Clear |
| Fundus | Within normal limits | Optic disc was pale with distinct margins, retinal pallor suggestive of central retinal artery occlusion. Cherry red spot along with edema was seen in macular region [Figure 1]. |
| On ocular coherence tomography | Within normal limits | Raised macular contour (7.15 µm) with central serous retinopathy [Figure 2]. |
The hematological investigations were – hemoglobin –6.7 g/dL; hematocrit –20.7%; platelets –150 × 103/uL; and white blood cell –3.18 × 103/uL. Liver function tests, blood glucose, urea, serum creatinine, and electrolytes were normal. The CT scan finding appeared normal. Hemoglobin high-performance liquid chromatography (HPLC) reports of patient along with her parents and siblings were done. Both parents report showed sickle cell trait pattern (father HbS –31.1% [Figure 3]; mother HbS – 27.6% [Figure 4] of graph area %) in HPLC test. The patient (daughter) report showed homozygous sickle cell (HbS –76.1% of graph area %) [Figure 5].
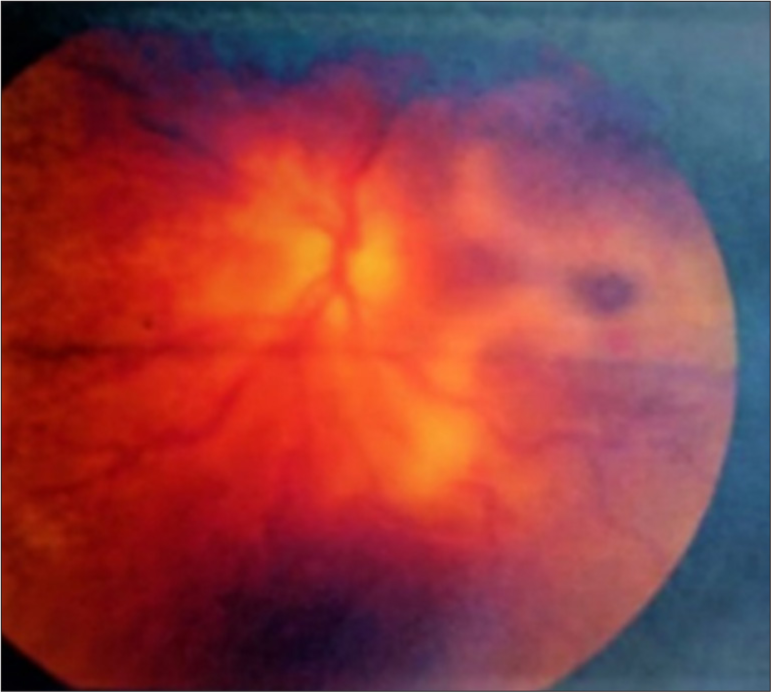
- On fundus examination, optic disc was pale with distinct margin with cherry red spot.
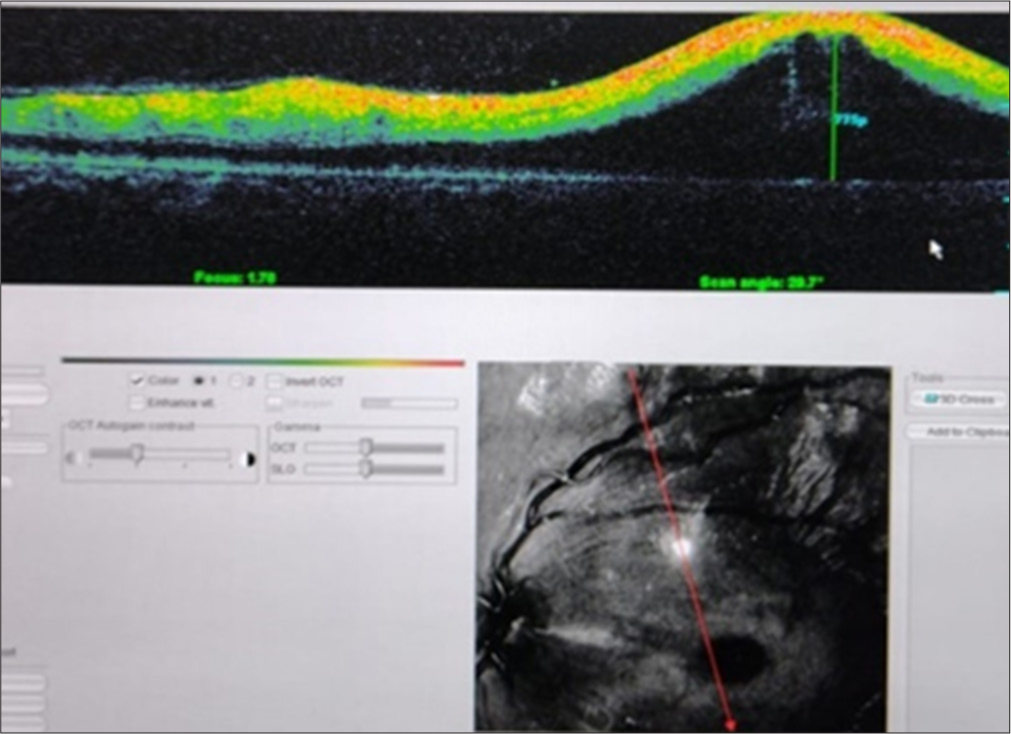
- Ocular coherence tomography showing raised macular contour (7.15 µm).
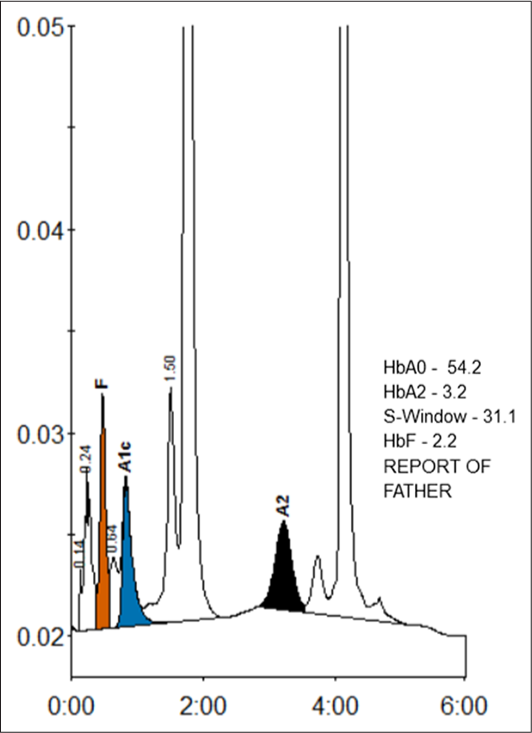
- HPLC report showing S-window – 31.1% of area % of graph.
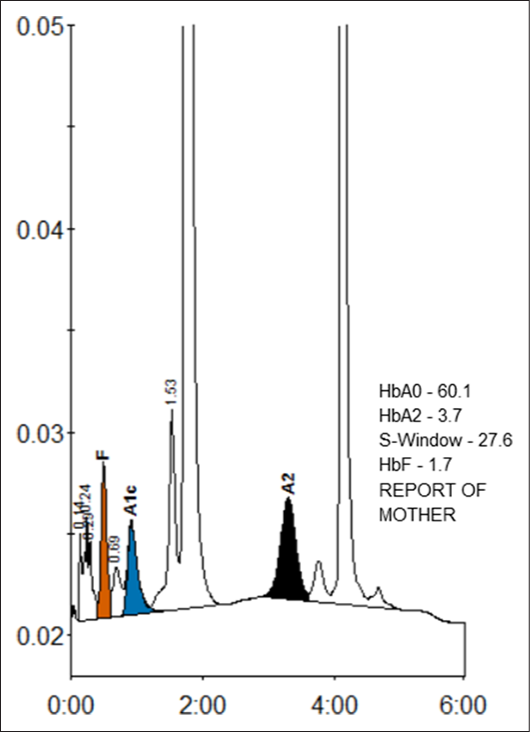
- HPLC report showing S-Window – 27.6% of area % of graph.
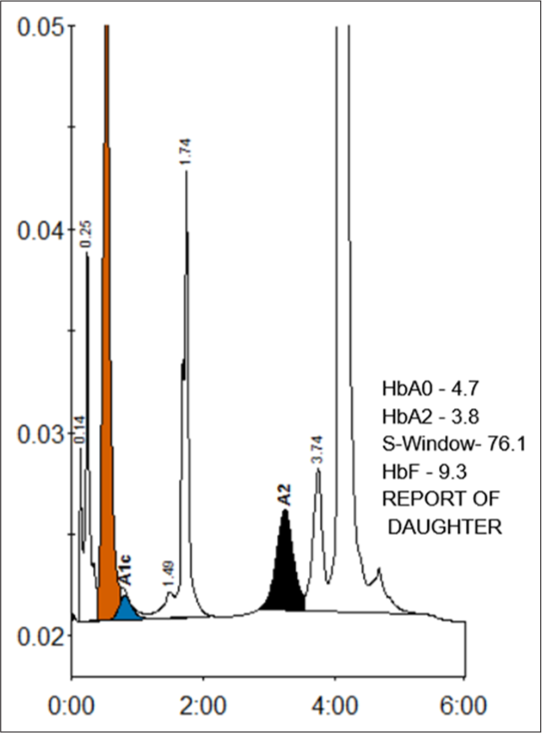
- HPLC Report showing S-Window – 76.1% of area % of graph.
DISCUSSION
SCA causes structural changes in hemoglobin which leads to formation of sickled shaped red blood cell. Then, polymerization of sickle red blood cell leads to the development of vaso-occlusion. Sickle cell vaso-occlusive events can affect vascular bed of different organs in our body. In eyes, it may leads to devastating visual consequences.[4] The pathogenesis of retinopathy in SCD is sequential events of hypoxia, acidosis, and ischemia promotes angiogenesis and this may subsequently result in retinal complications. According to Goldberg’s classification,[5] these stages are as follows:
Stage I: Peripheral arterial occlusion which is caused by the aggregation of sickled hemoglobin,
Stage II: Polymerization leads to peripheral arteriovenous anastomosis,
Stages III: Anastomosis form sea-fan appearance area due to neovascularization,
Stage IV: This neovascularization leads to vitreous hemorrhage, and
Stage V: These events cause tractional retinal detachment.
CRAO is the occlusion of central retinal artery that supplies the innermost layer of the retina. Acute CRAO is an emergency condition that may lead to severe to permanent visual loss in more than 90% of cases. According to the ophthalmological guidelines, these cases require immediate intervention to save the vision. These interventions are treatment with acetazolamide, ocular massage, blood transfusion (low Hb), and selective ophthalmic artery catheterization with thrombolytic agents or intravenous fibrinolytic therapy. Meta-analysis of intravenous fibrinolytic therapy in CRAO showed a recovery rate of up to 30%, if done within the first 4.5 h after onset of symptoms. Pikija et al. explained that CRAO affected patients may benefitted from the intravenous recombinant tissue plasminogen activator therapy, if done timely.[6]
This case was represented with complain of loss of vision from the past 3 days. On ophthalmological evaluation, the patient showed signs of both stage III and IV sickle cell retinopathy. CRAO was diagnosed fundus examination. As the case had been presented after 3 days of appearance of symptoms, the prognosis was poor. The patient had been counseled and prescribed higher dose of hydroxyurea (500 mg BD twice daily) to prevent further vaso-occlusive complications.
A study stated that CRAO may be also seen in SCA as well as in sickle cell trait patients also.[7] Studies indicate that peripheral vaso-occlusion may be observed as early as 20 months of age, clinically detectable retinal disease is found most commonly between 15 and 30 years of age.[8]
CONCLUSION
SCD should be considered as a significant risk for CRAO. Early stages of sickle cell eye disease do not usually result in visual symptoms, so, the disease can go undetected unless a formal eye examination (slit lamp and fundus evaluation) is performed by an ophthalmologist. The general and systemic examination should include an accurate measurement of visual acuity, assessment of papillary reactivity, careful evaluation of the anterior structures of the eye using a slit-lamp biomicroscope, and a thorough examination of the posterior and peripheral retina through a dilated pupil. Early diagnosis of patients by periodic screening along with the early evaluation for complication is very important to prevent the visual complication. Patients with their parents should be given genetic counseling and treatment support timely. There should be frequent special health camps for screening of disease in prone regions. Awareness programs with sensitization for disease must be introduced, so early detection, timely counseling with treatment can be done.
Ethical approval
The research/study approved by the Institutional Review Board at ISPAT general hospital, number IEC/IGH/2024/23, dated 11th March, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Retinal occlusion as an advanced complication of sickle cell disease. New Front Ophthalmol. 2016;2:1-7.
- [CrossRef] [Google Scholar]
- Concurrent bilateral central retinal artery occlusion secondary to sickle cell crisis. J Investig Med High Impact Case Rep. 2021;9:23247096211028392.
- [CrossRef] [PubMed] [Google Scholar]
- The incidence of central retinal artery occlusion in Olmsted County, Minnesota. Am J Ophthalmol. 2011;152:820-3.e2.
- [CrossRef] [PubMed] [Google Scholar]
- The management of sickle cell disease In: NIH publication No. 2-2117. Bethesda: National Institute of Health; 2002.
- [Google Scholar]
- Classification and pathogenesis of proliferative sickle retinopathy. Am J Ophthalmol. 1971;71:649-65.
- [CrossRef] [PubMed] [Google Scholar]
- Central retinal artery occlusion in a patient with sickle cell disease treated with recombinant tissue plasminogen activator. Folia Med (Plovdiv). 2022;64:840-3.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous central retinal artery occlusion in a teenager with sickle cell trait. Middle East Afr J Ophthalmol. 2015;22:119-21.
- [CrossRef] [PubMed] [Google Scholar]
- Dual perspective analysis of vascular formations in sickle retinopathy. Arch Opthalmol. 1993;111:1234-45.
- [CrossRef] [PubMed] [Google Scholar]






