Translate this page into:
Cryptococcus of bone marrow – A case report in non-HIV and non-Hodgkin’s lymphoma patient
*Corresponding author: Sudha Madhuri Kandikanti, Department of Pathology, Care Hospitals, Hyderabad, Telangana, India. kandy_sudharhea@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Kandikanti SM, Koppaka DK, Byreddy PR. Cryptococcus of bone marrow – A case report in non-HIV and non Hodgkin’s lymphoma patient. J Hematol Allied Sci. doi: 10.25259/JHAS_3_2025
Abstract
Infections are an important cause of morbidity and mortality in non-Hodgkin’s lymphomas (NHLs). Factors contributing to increased risk of infection include the nature of the underlying disease itself as well as treatment-induced immunosuppression. Disseminated cryptococcosis is predominantly seen in human immunodeficiency virus-infected people and less commonly seen in individuals with preserved immune function. Other conditions that suppress the host immunity such as hematologic malignancies, organ transplantation, and immunosuppressive drugs are implicated as risk factors. Most commonly, it affects the lungs, followed by the central nervous system, skin, and bone marrow. Here, we present a case of Cryptococcus in a known and treated case of NHL, presented with seizures, vomiting, headache, and fever. Bone marrow examination clinched the diagnosis which showed diffuse infiltration by atypical lymphoid cells along with extracellular encapsulated yeasts which were variably sized with narrow-based budding.
Keywords
Bone marrow
Cryptococcus
non-Hodgkin’s lymphoma
INTRODUCTION
Cryptococcosis is a rare fungal infection that can affect the bone marrow of patients with non-Hodgkin lymphoma (NHL): Cryptococcus neoformans can affect almost any organ in severely immunosuppressed people, including the bone marrow. The most common risk factors for cryptococcosis in patients with cancer are impaired cell-mediated immunity and high doses of steroids. In one study, NHL had the highest incidence rate of cryptococcosis among hematological malignancies (HMs), with 7.35 cases/1000 NHL patients.[1] Cryptococcosis commonly presents with pulmonary, central nervous system (CNS), or skin involvement. Bone marrow involvement of cryptococci has been rarely reported.[2]
CASE REPORT
A 45-year-old female was diagnosed with NHL and the subtype was not categorized upfront at an outside hospital. The patient received six cycles of chemotherapy and end-of-treatment computed tomography scan revealed no evidence of disease. The patient presented 8 years after diagnosis with seizures. She was admitted for reeling sensation, seizures, vomiting, headache, and fever at other center. Peripheral smear revealed atypical lymphoid cells for which bone marrow was performed and sent to flow cytometric analysis. Bone marrow was infiltrated with atypical lymphoid cells. Flow cytometry revealed CD 5 and CD 23-positive malignancy favoring chronic lymphocytic leukemia with Matutes score 4. As the condition worsened, she was referred to our center for further management. Magnetic resonance imaging brain and spine was done which revealed meningeal enhancement suspicious of lymphoid infiltrates. Cerebrospinal fluid (CSF) flow cytometry revealed monoclonal B-cell infiltrates. Gram stain and acid–fast bacteria stain on CSF were negative. The patient was started on IV rituximab.
Re-aspiration of bone marrow along with trephine biopsy was performed and analyzed. Bone marrow examination revealed diffuse infiltration by atypical lymphoid cells. Also were seen extracellular encapsulated yeasts which were variably sized with narrow-based budding [Figure 1]. This finding was further confirmed by performing special stain – Grocott’s methenamine silver (GMS) which highlighted capsulated yeasts [Figure 2]. The patient was started on amphotericin and flucytosine. Immunohistochemical studies were planned on trephine biopsy to categorize the type and the nature of lymphoid infiltrate but the patient succumbed to death.
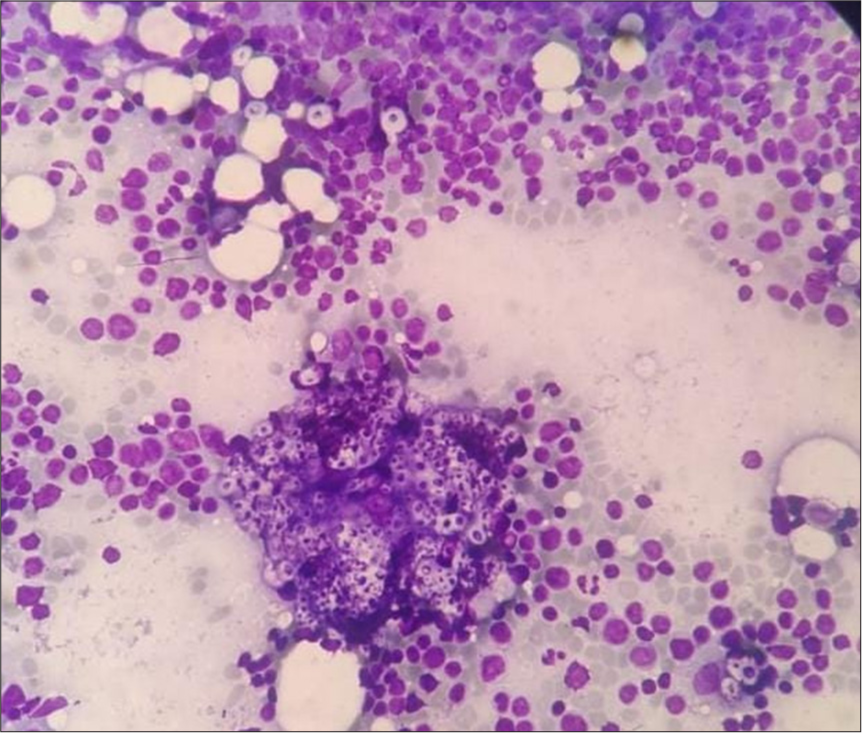
- Bone marrow revealing extracellular variably sized encapsulated yeasts with narrow-based budding along with adjacent atypical lymphoid infiltrate, Geimsa, ×400.
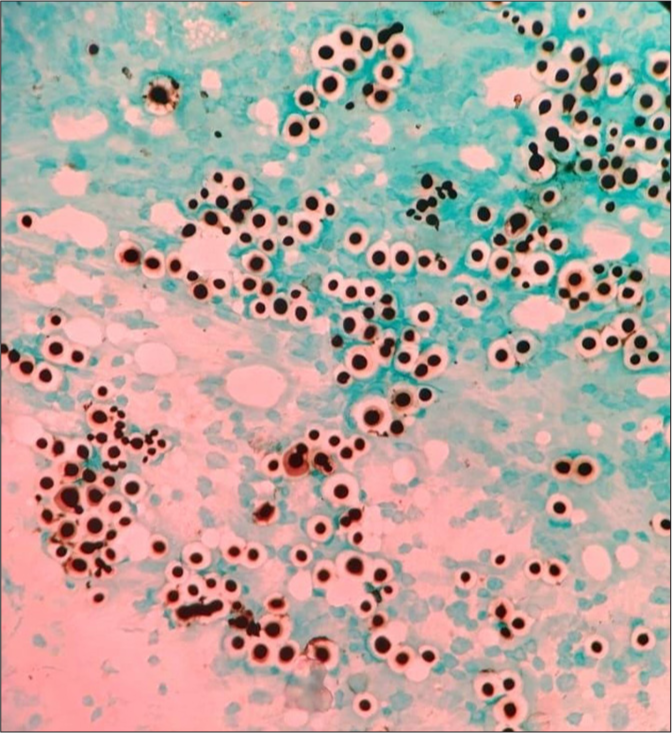
- Special stain highlighting the fungi, Grocotts methamine silver stain, ×400.
DISCUSSION
Cryptococcus is the most common cause of morbidity and mortality in immunocompromised individuals and it is the second most common fungal infection which is seen in acquired immunodeficiency syndrome (AIDS). Cryptococcus commonly presents with involvement of pulmonary, CNS, or skin. Prostatic, hepatic, and bone marrow involvements are rarely reported.[3,4]
Only very few cases of cryptococcosis of bone marrow are reported and its exact incidence is not known. The diagnosis can be established by growth obtained in culture, by biochemical analysis, or by an examination of the tissue with special stains like GMS or periodic acid–Schiff or mucicarmine positivity or serologically by polysaccharide capsular antigen detection.[5].
Bone marrow examination plays a crucial role in detecting opportunistic fungal infection like cryptococcosis for the evaluation of pancytopenia in immunosuppressed individuals seen on aspirate, but trephine biopsy of bone marrow shows numerous clusters of cryptococci, which stresses the significance of performing trephine biopsies along with the bone marrow aspiration procedure. The presence of cryptococci in the aspirate in the absence of granulomas is an unusual finding as was our case. Cryptococcus has a gelatinous polysaccharide capsule which can result in a gelatinous mass or a pseudocyst formation, with many clusters of cryptococci within the pool of mucin.[6]
The most common presentation of cryptococcal infection is subacute meningitis, especially when CD4+ T lymphocyte count is below 100 cells/μL. This was also a presenting symptom in our case. However, in severely immunocompromised individuals, Cryptococcus can infect virtually any organ, and bone marrow involvement is a rare presentation of cryptococcosis.[7]
During the study done by Meza et al. in individuals with HMs, cryptococcosis has an incidence rate of 47.6% in NHL, 23.8% in acute leukemias, 19.1% in multiple myeloma, and 9.5% in Hodgkin lymphoma. The sub-group analysis showed that NHL has the highest incidence rates followed by multiple myeloma.[1]
In a retrospective study by Wang et al., CNS cryptococcal infection was more common in patients with hematological non-malignancies, and serologically cryptococcal antigen test as well as fungal culture of CSF or Indian ink smear preparation for early detection and diagnosis are suggested.[8] T-cell lymphocyte subset population are often involved in the defense against fungal infections. Persons with T-cell dysfunction, such as in human immunodeficiency virus (HIV), induction chemotherapy for bone marrow transplant, proteasome inhibitor therapy, are at increased risk for cryptococcosis. Our case was HIV negative, status of which was confirmed twice. Treatment is difficult task because of emerging resistance to antifungal drugs. Cryptococcosis often requires the use of combination of many antifungal drugs, including fluconazole, liposomal amphotericin B, and flucytosine[9] and our case was also treated with last two drugs.
Apart from HIV infection, immunosuppressive drugs, hematologic malignancy, post-organ transplantation, rheumatologic disorders, and chronic organ failure can also predispose individuals to this infection.[10] Factors contributing to the increased risk of infection in these individuals include the nature of the underlying disease itself, as well as treatment-induced immunosuppression[11] as our case. It requires high index of clinical suspicion and prompt initiation of antifungal therapy to treat these patients.
Furthermore, this case highlights the risk of Cryptococcus fungal infection in immunocompromised conditions other than HIV/AIDS, stressing the necessity of considering this diagnosis when physicians encounter an opportunistic neuroinfection.
CONCLUSION
Physicians need to be aware that cryptococcal meningoencephalitis can be possible diagnosis in patients with hematological malignancies presenting with neurological symptoms. It requires high index of suspicion, prompt diagnosis with serological and relevant tests including bone marrow examination to look for capsulated fungi. Treatment with at least two antifungal agents should be initiated as soon as possible since cryptococcal meningoencephalitis can have fatal consequences.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cryptococcosis in non-HIV/non-transplant hematological patients: A 12-year retrospective clinical analysis in a Peruvian referral cancer center. J Clin Oncol. 2023;41:e19536.
- [CrossRef] [Google Scholar]
- Cryptococcososis of bone marrow: A case report with review of literature. J Clin Diagn Res. 2014;8:158-9.
- [Google Scholar]
- Cryptococcal granulomas in an immunocompromised HIV-negative patient. Indian J Pathol Microbiol. 2008;51:553-5.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated cryptococcosis mimicking lymphoreticular malignancy in a HIV negative patient. JK Sci. 2004;6:93-5.
- [Google Scholar]
- Cryptococcal neoformans profiles in peripheral blood neutrophils: An unusual presentation. Indian J Pathol Microbiol. 2008;51:296-7.
- [CrossRef] [PubMed] [Google Scholar]
- Choroid plexitis as a mass lesion: MR imaging and histopathologic correlation. AJNR Am J Neuroradiol. 2002;23:273-6.
- [Google Scholar]
- Invasive fungal infection by Cryptococcus neoformans var. grubii with bone marrow and meningeal involvement in a HIV infected patient: A case report. BMC Infect Dis. 2019;19:220.
- [CrossRef] [PubMed] [Google Scholar]
- Cryptococcosis in patients with hematological diseases: A 14-year retrospective clinical analysis in a Chinese tertiary hospital. BMC Infect Dis. 2017;17:463.
- [CrossRef] [PubMed] [Google Scholar]
- Cryptococcal meningoencephalitis, 10 years after bone marrow transplant in a patient with multiple myeloma. Cureus. 2020;12:e12094.
- [CrossRef] [Google Scholar]
- Cryptococcosis in human immunodeficiency virus-negative patients in the era of effective azole therapy. Clin Infect Dis. 2001;33:690-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Description of the type, frequency and severity of infections among sixteen patients treated for T-cell lymphoma. J Hematol. 2021;10:123-9.
- [CrossRef] [PubMed] [Google Scholar]






