Translate this page into:
Bone infarct (osteonecrosis) as late side effect of steroid in acute lymphoblastic leukemia survivor
-
Received: ,
Accepted: ,
How to cite this article: Shekhawat PS, Garg M, Dolai TK. Bone infarct (osteonecrosis) as late side effect of steroid in acute lymphoblastic leukemia survivor. J Hematol Allied Sci 2021;1(1):38–40.
Abstract
Survivors of acute lymphoblastic leukemia (ALL), though cured of their primary disease may suffer from long-term complications such as bone infarction contributing to a major morbidity. Here, we report a very rare case of bone infarct in bilateral tibia and femur of a patient of acute lymphoblastic leukemia, post completion of maintenance chemotherapy. With this case report, we suggest that appropriate preventive measures are necessary to decrease the risk of this very rare morbidity.
Keywords
Osteonecrosis
Bone infarct
Acute lymphoblastic leukemia
ALL survivor
Steroid
INTRODUCTION
Osteonecrosis is a disease in which death of cellular elements of bone occurs as a result of diminished arterial blood supply. Immunologic factors, vasculitis, disease-associated features, as well as antiphospholipid antibodies, and prolonged use of corticosteroids have been implicated in the development of osteonecrosis.[1] Bone infarction is a term referring to osteonecrosis that involves metaphyseal or diaphyseal region of long bones.[2,3]
Here we present a very rare case of bone infarct in bilateral tibia and femur of a patient of acute lymphoblastic leukemia, post completion of maintenance chemotherapy.
CASE REPORT
A 19-year-old euthyroid, non-diabetic, acute lymphoblastic leukemia (ALL) survivor female presented to survival clinic (> 2 year after completing therapy) of hematology department for her annual checkup with complaints of constant dull aching pain in bilateral lower limbs for 8 months, which was insidious in onset and gradually progressive. She was being treated with calcium and pain killers by a local physician but all in vain. She was diagnosed with pre–B ALL, IRG in August 2014 and was treated with BFM 90 protocol without cranial radiotherapy. She finished her reinduction therapy in March 2015 and completed her maintenance chemotherapy in September 2017. Since then, her disease was in remission.
She was fully evaluated with complete blood counts with peripheral smear for disease status and biochemical parameters along with liver function test, lipid profile, serum calcium, vitamin D3 and serum phosphate levels. All the above parameters were within normal limits. X ray of bilateral lower limbs including tibia and femur was advised and it showed hyper dense opacities in bilateral tibia and femur suggestive of infective changes. Non-contrast MRI scan of bilateral lower limbs was done which revealed bilateral symmetrical abnormality in the medulla of the proximal tibia involving metaphyseal region with central area of fat signal surrounded by serpiginous T1 and T2 hypointense rim as shown in Figure 1A. There was T2/STIR hyperintensity surrounding the central lesion as shown in Figure 1B. The overlying cortex was intact with no periosteal reaction. Similar changes were noted in the medullary cavity of shaft of femur on both sides and distal tibial shaft on left side. Overall, the features were suggestive of bilateral bone infarct in tibia and femur. She is being managed with analgesics in view of nonsurgical approach advised by orthopedic team and no new similar lesion appeared till her last survival clinic follow up in March 2021.
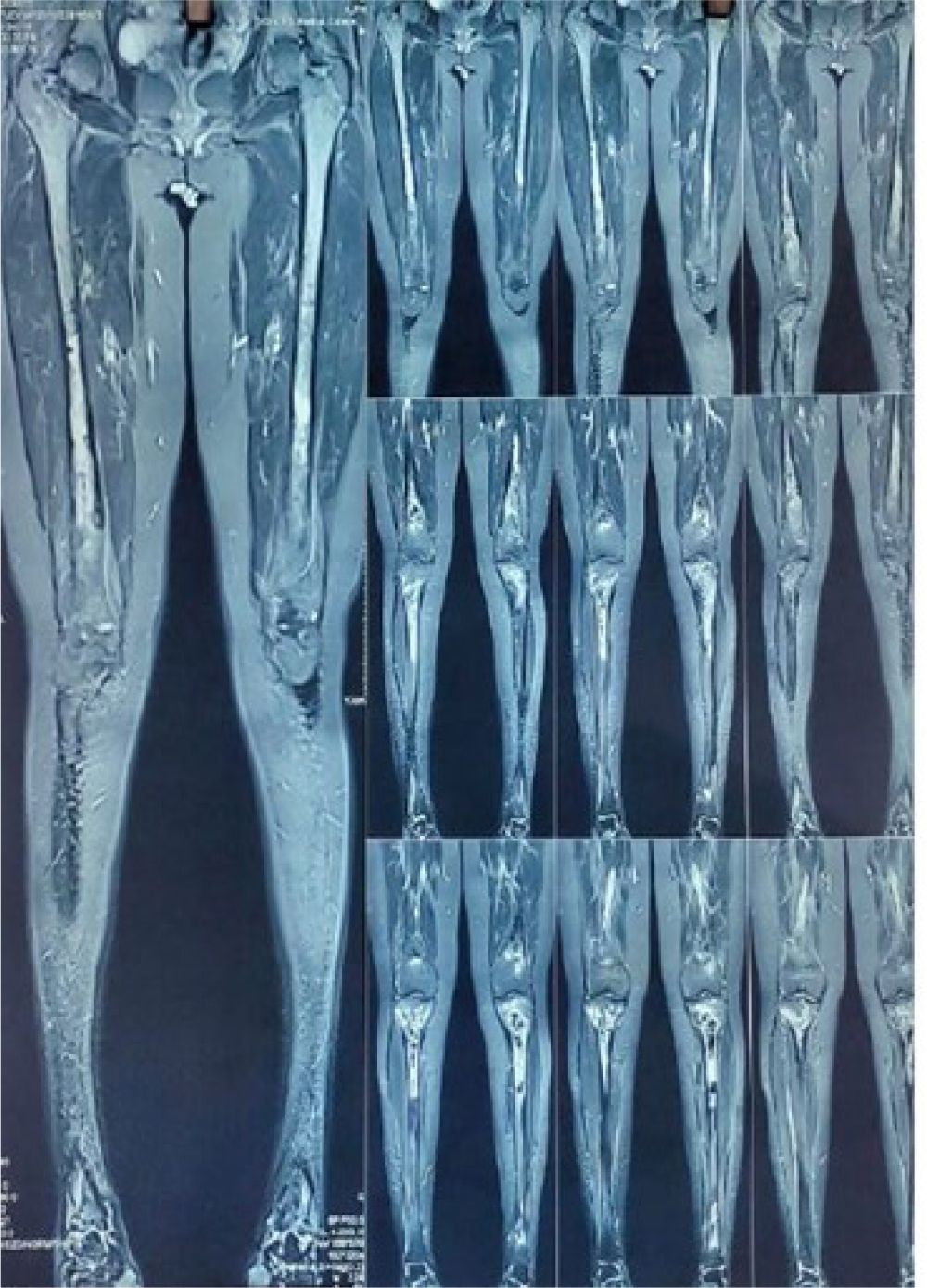
- Shows coronal view of both lower limbs showing bilateral bone infarct of distal femur and proximal tibia.

- Shows sections showing bilateral tibial T2/STIR hyperintensity surrounding the central lesion.
DISCUSSION
Corticosteroids are given as a standard treatment of acute lymphoblastic leukemia. These patients though cured with the disease, may suffer from long-term complications of the treatment and one such complication being non-traumatic osteonecrosis. Though there are very limited reported cases of the same, bone infarction being even rarer, it contributes to a major morbidity in ALL survivors.
Brooker et al.[4] have reported a case bilateral hip, shoulder, and knee osteonecrosis following high dose corticosteroid therapy for dermatomyositis, Brien et al.[5] have reported case of multifocal osteonecrosis after 2-week course of methylprednisolone for treatment of septic shock. Rottoli et al.[6] have reported two cases of symptomatic avascular necrosis of distal femur in two multiple sclerosis patients after use of methylprednisolone. There are several studies where cases of osteonecrosis following corticosteroids have been reported,[3-6] however cases of bone infarction and that too in ALL survivors is only rarely reported.
In a review article by Weldon,[7] hyperlipidemia, alcoholism, smoking, connective tissue disorders, and/or previous trauma to the affected area have been highlighted as few of the major risk factors contributing to osteonecrosis in patients on corticosteroids. The pathogenesis of corticosteroid induced osteonecrosis is multifactorial and still debated, hyperlipidemia and/or micro fat emboli, being identified as few of the pathogenic mechanisms.[4,7]
Osteonecrosis causes severe pain and hampers the quality of life of these patients. As surgical intervention is warranted in treatment of osteonecrosis, appropriate preventive measures are necessary to decrease the risk of this morbidity. Proper exercise and early recognition of the risk factors play an important part in prevention.
CONCLUSION
Survivors of ALL, though cured of their primary disease may suffer from long-term complications such as bone infarction contributing to a major morbidity. Hence, such rare complication must be kept in mind. Early recognition of risk factors and timely preventive measures may decrease the chances of osteonecrosis in these patients.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Immunologic factors in the pathogenesis of osteonecrosis. Orthop Clin North Am. 2004;35:259-63.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral knee pain associated with bone infarction in a patient with Behcet's disease. Case Rep Rheumatol. 2012;2012
- [CrossRef] [PubMed] [Google Scholar]
- Osteonecrosis and bone infarction in association with Behcet's disease: report of two cases. Clin Exp Rheumatol. 2001;19(5; SUPP/24):S-51.
- [Google Scholar]
- Osteonecrosis: The perils of steroids. A review of the literature and case report. Case Rep Clin Med. 2012;1:25-36.
- [Google Scholar]
- Multifocal osteonecrosis after short-term high-dose corticosteroid therapy. A case report. Clin Orthop Relat Res 1992:176-9.
- [CrossRef] [PubMed] [Google Scholar]
- Steroid induced femoral osteonecrosis in multiple sclerosis: two case reports. SM Musculoskelet Disord. 2017;2:1019.
- [CrossRef] [Google Scholar]
- The effects of corticosteroids on bone: osteonecrosis (avascular necrosis of the bone) Ann Allergy Asthma Immunol. 2009;103:91-7. quiz 97-100, 133
- [CrossRef] [PubMed] [Google Scholar]






